The State of Surgery as a Career in 2025
Max Schloemann2024-12-23T18:42:44+00:00The field of surgery continues to evolve rapidly, influenced by shifting patient demographics, advancements in medical technology, and a growing demand for surgical interventions. In response to years of healthcare workforce shortages, the national employment landscape shows promise for surgeons, and recent data confirms that surgical specialties correspond to high demand, high salaries, and a high impact on public health.
This article explores the current landscape and future career prospects for surgeons in 2025, highlighting the multifaceted professional benefits and opportunities and the challenges and liabilities associated with surgery.
What Do Surgeons Do?
Where Do Surgeons Work?
According to the American College of Surgeons, standard workplace settings for a surgeon include:
- Hospitals
- Academic Medicine
- Private Practice
- Ambulatory Surgery Centers
- Contract Assignments through a Staffing Agency
- Institutional Practice
- Government Service Programs
- Military/Uniformed Services
Professional Advantages for Surgeons in 2025
After years of extensive education and training, surgeons offer an incredibly complex and rare skillset that saves lives every day. As such, surgeons play a crucial role across the healthcare sector and have access to many professional benefits.
For 2025 and beyond, the favorable outlook for surgeons predicates upon these contributing factors:
- Growing Market Value in the U.S.
Based on the 2023 market size of $830 Billion, experts predict that the U.S. surgical procedures market will surpass $1 trillion around 2027 and climb to $1.52 trillion by 2033.
These market growth predictions indicate that surgeons will have considerable flexibility and autonomy with employment opportunities in response to the high demand for their expertise.
Surgical procedures in the United States are expected to reach a $930 Billion market value in 2025 and $1.52 Trillion by 2033.
Source: Precedence Research
- Increasing Demand for Surgery
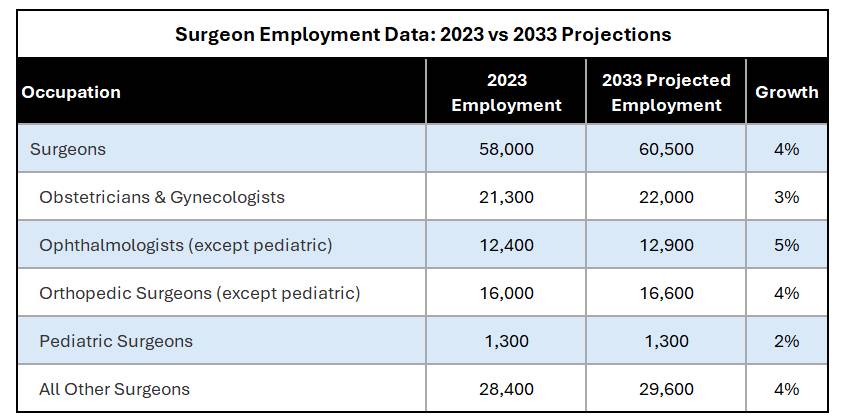
According to the U.S. Bureau of Labor Statistics, surgeon employment is projected to increase by 4% between 2023 and 2033. The projected growth rate varies among specialties, as illustrated by the chart below:Projected employment growth rates for surgeons through 2033 range from 2-5% depending on subspecialty.
Source: U.S. Bureau of Labor StatisticsWhy is the Demand for Surgeons Increasing?
One of the most significant factors generating demand for surgeons is the aging global population, which correlates with increasing healthcare needs. In the U.S., this is primarily due to the predominance of the Baby Boomer generation in both the medical workforce and patient population.
Key contributing factors:
- Aging General Population
According to the World Health Organization, the number of people aged 60 or older will increase by 34% from 2020 to 2030. An older population typically requires more surgical interventions, including orthopedic hip and knee replacements, interventional cardiology, and cataract surgeries. This explains why ophthalmologists’ and pediatric employment projections have the highest and lowest expected growth rates, respectively. - Aging Surgical Workforce
Physicians aged 65+ currently represent 20% of the clinical physician workforce, and a significant portion will exit within the next decade. As more Baby Boomer surgeons reach retirement age, the Association of American Medical Colleges (AAMC) projects that the U.S. will face a physician shortage of up to 86,000 providers by 2036.Looking specifically at AAMC surgical provider data, by the end of 2022, 25.6% of surgeons were older than 65 years. That percentage is even higher for the subspecialties of Ophthalmology, Orthopaedic, Plastic, Thoracic, and Urology.This impending gap signifies ample growth opportunities for new surgeons entering the field and a potential avenue into leadership roles for experienced surgeons.The dark blue bar represents surgeons 65+ compared to their younger counterparts for every surgical specialty except Sports Medicine.
Source: American College of Surgeons -
Expanded Patient Access
In response to the COVID pandemic, telemedicine infrastructure and acceptance within healthcare strengthened rapidly and continue to impact patient access today. Surgeons can now offer remote patient consultations to a broader population. Specialist healthcare teams are no longer bound by geography, encouraging virtual multidisciplinary collaboration to help patients anywhere in the country.
Some local governments and healthcare organizations have offered incentives to attract and retain surgeons, such as scholarships, loan forgiveness, and relocation or housing support, to improve healthcare accessibility in underserved regions further.
- Aging General Population
-
Groundbreaking InnovationsAs advancements in medical technology continue to flourish, surgeons will have exciting new methods and protocols to explore in 2025. Many of these innovations offer high-precision, minimally invasive approaches that have the potential to reduce patient recovery time and mitigate medical malpractice risk for providers.
Examples include:-
Robotic Surgery
Robotic systems, such as the widely popular da Vinci Surgical System, allow for smaller incisions, greater precision, and faster patient recovery times.
-
Artificial Intelligence
AI algorithms can assist surgeons with preoperative planning, interpretation of patient imaging, and real-time analytics or navigation assistance during an operation, potentially reducing surgery time and improving efficiency.
-
Virtual & Augmented Reality (VR & AR)
VR simulators create a realistic training environment for surgeons that poses zero risk to human patients. Studies have shown that VR training can improve procedural accuracy compared to traditional methods, leading to better patient outcomes and reduced liability risk for the surgeon.
In the operating room, AR overlays of patient data and 3D anatomical models can be projected directly onto the surgery site, helping surgeons make accurate, data-driven decisions in real time.
-
-
High Earning PotentialAccording to the Medscape Physician Compensation Report 2024, surgeons remain among the highest-paid healthcare providers due to their specialized skills and high level of responsibility. However, individual salaries vary based on specialty, years of experience, and geography.
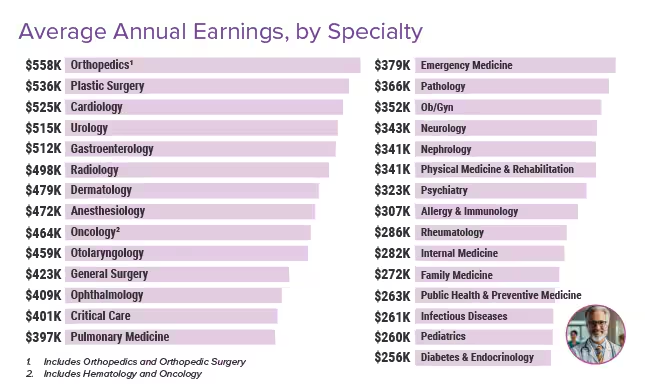 Orthopedics, Plastic Surgery, Cardiology, Urology, and Gastroenterology ranked as the top 5 specialties according to average annual earnings.
Orthopedics, Plastic Surgery, Cardiology, Urology, and Gastroenterology ranked as the top 5 specialties according to average annual earnings.Source: 2024 Medscape Physician Compensation Report
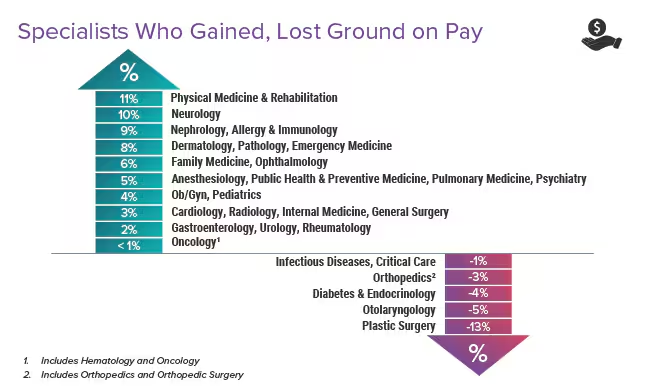
Specialist compensation gains ranged from +11% to -13%.
Source: 2024 Medscape Physician Compensation ReportHighlights from the 2024 report include:
- Surgical salary growth outpaces nonsurgical salaries.
Between 2022 and 2023, total compensation for surgical specialists increased by 4.4%, while nonsurgical specialist compensation rose by less than 2%. - Orthopedic surgeons are the highest-paid subspecialty.
Subspecialties like orthopedic surgery and plastic surgery command the highest salaries, followed closely by general surgeons, OB/GYNs, and neurosurgeons. - Salary trends differ based on specialty.
Though plastic surgeons earn the second highest average salary, the specialty experienced the largest downward trend, 13%. - Local demand and competition levels impact earning potential.
Surgeons are well-compensated in underserved regions with high demand and low competition, though urban hubs also offer high salaries due to cost of living levels.
- Surgical salary growth outpaces nonsurgical salaries.
Source: 2024 Medscape Physician Compensation Report
Professional Challenges for Surgeons in 2025
In 2025, in addition to the inherent challenges of a demanding career in healthcare, surgeons will potentially face obstacles related to recent industry trends, regulatory changes, and malpractice litigation precedents.
-
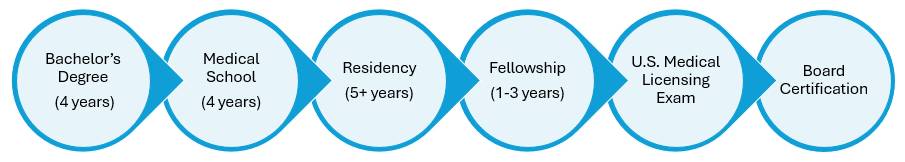
- Rigorous Commitment
Becoming a surgeon is long and hard, requiring intense time commitments and deep financial investments to obtain the necessary education, training, and credentials.Surgeons typically follow this process before they can practice medicine independently:
Board-certified surgeons dedicate 14+ years to their training and education.A commitment of this length and vigor requires personal sacrifice, often at the cost of work/life balance during the most intense phases. However, emerging trends such as mentorship programs, loan forgiveness policies, and VR-assisted training programs show promise for revolutionizing the process.
- Disruptive Regulatory Changes
State and federal regulatory policies focusing on patient safety, quality of care, and financial reimbursement are influencing surgical practice in a variety of ways, such as:- Value-Based Care Payment Model
As the fee-for-service model shifts to a value-based care model that directly links reimbursement amounts with patient outcomes, surgeons are held more accountable for the safety and quality of their care. - Reproductive Care
For OB/GYNs surgeons specifically, abortion-legislation can complicate patient care as well as liability exposure depending on the state in which they practice. As such, OB/GYNs must navigate a complex and evolving situation to minimize professional liability while delivering safe, compliant care to pregnant women.According to the March of Dimes, a maternal and infant health non-profit, OB/GYN shortages are more pronounced in states that prohibit abortion in comparison to states where abortion is less regulated, leaving 1 in 3 U.S. counties with enough obstetric surgeons to provide maternal care.For OB/GYNs in the less-regulated states, this can lead to an increase in out-of-state and remote patients, which requires careful attention to state legal requirements and malpractice coverage parameters. - Decreased Medicare Reimbursements
For the 5th year, the Centers for Medicare and Medicaid Services (CMS) has decreased the conversion factor for Medicare physician reimbursement. Effective January 1, 2025, surgeons will be subject to a 2.83% cut to Medicare reimbursement payments, bringing the total decrease to 10% since 2020.
- Value-Based Care Payment Model
- High-Risk, High-Liability Field
The medical malpractice statistics of 2024 demonstrate the high liability landscape for surgeons:- Surgical errors account for 25% of all negligent provider claims.
- Surgeons are most likely to be sued for malpractice.
- High-risk specialties are most vulnerable to medical malpractice claims and lawsuits:
- OB/GYNs
- Neurosurgeons
- Bariatric Surgeons
- Orthopedic Surgeons
- Plastic Surgeons
- General Surgeons
- Rigorous Commitment
Malpractice insurance premiums are expected to keep climbing in 2025.
Projected rate increases reflect the substantial risks of surgery and recent escalations in legal defense fees, social inflation, and nuclear payouts.
Safeguard Your Career with Premier Liability Coverage
SURGPLI brokers specialize in finding affordable, robust coverage for surgeons in high-risk specialties who are often targets for medical malpractice lawsuits.
By securing comprehensive malpractice insurance coverage, surgeons can focus on helping patients address the growing demand for surgical expertise without worrying about professional liability exposure.
Which insurance carrier offers the best rates for your location & specialty?
Find out now by contacting a SURGPLI broker for a free consultation & quote.
Email info@SURGPLI.com or call 800-969-1339 to speak with someone in our Illinois office.
Read the latest From SURGPLI
SURGPLI CEO Max Schloemann shares expert insights in White Coat Investor on how physicians can budget for tail insurance before retirement. Get the details.
The Doctors Company is a top-rated medical malpractice insurance carrier with an AM Best “A” rating and strong coverage options. Get a quote with SURGPLI today.
New abortion laws complicate OB/GYN liability. With shifting state laws impacting coverage, reviewing malpractice policies is more crucial than ever. Learn more.












Stay In Touch